Turning healthcare IT architecture inside out
In just a few years, conversations around the importance of data in healthcare have changed dramatically. We understand that accessible quality data is paramount to improving health and care. Still, it took a pandemic to cause a market shift, and providers are finally starting to think about data first and applications second.
We are seeing more and more procurements where the data formats are not left to the vendors. Instead, tenders are requesting solutions based on open, published, vendor-neutral data standards. Examples include national systems like Slovenia, Malta, Scotland, Finland, Wales, and recently Catalunya, and top institutions like Heidelberg, The Christie, and Karolinska.
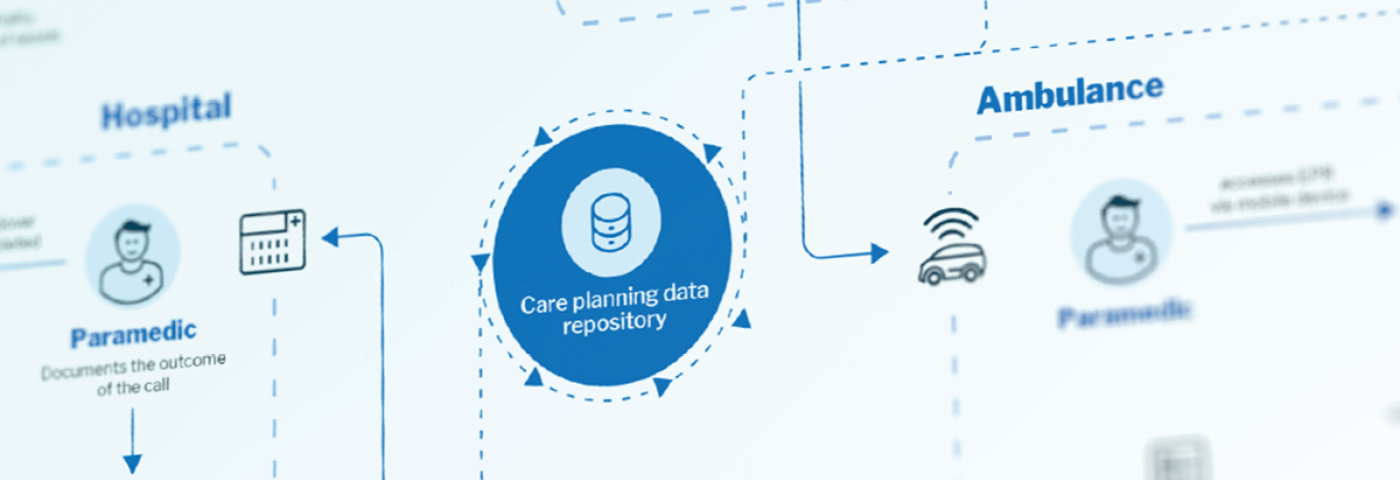
We are also seeing healthcare systems evolving, focusing on a more holistic approach to care. This involves bringing care closer to the citizen and coordinating care activities between different providers. The future of health and care does not revolve around provider organisations, but around the citizen. At the centre of that is a longitudinal care record providing a single source of truth.
Recognising this, some regions are starting to take a different approach. Instead of capturing data locally and then sharing some of it centrally, they begin with a shared care record, build applications on top, and then push the applications out to the providers in the region. To ensure ease of use, centrally managed components are embedded within provider systems using contextual launch and single-sign-on. Alternatively, a centrally managed portal is used in low-acuity environments like care homes, where providers often lack adequate systems. This approach automatically creates a patient-centric care record, simplifies governance of data formats and terminologies, and speeds up application distribution and updates immensely.
As current approaches to interoperability provide lacklustre results, we need to rethink the architecture of health IT. Today providers capture health data in various systems using proprietary data formats, sending some data to regional shared care records. New architectures have a vendor-neutral data layer at the centre and low code tools to accelerate delivery by pushing application functionality to provider systems. This facilitates care coordination and provides a single source of truth, keeping everyone on the same page, including the patient. After all, care records should serve the patient and provider organisations. In that order.
You can read the whole blog post from Tomaž Gornik here: Turning healthcare IT architecture inside out.