ehealth
How did Slovenia modernise its eHealth system?
Slovenia's national eHealth system has played a crucial role in modernising healthcare practices and improving patient care. However, as the system evolved over the years, it has become apparent that several limitations hinder its full potential. In response to these challenges, Slovenia is embarking on a comprehensive eHealth system upgrades project that promises to revolutionise how healthcare information is accessed, managed, and utilised.
The Slovenian Ministry of Health (MoH) transitioned from an exchange-based model to a platform-based architecture, emphasising the core principle that data is essential to healthcare. This shift involved separating standardised data management from individual applications, allowing for the adoption of national-level, patient-centered data models. The CRPD platform now excels in interoperability, fostering a multi-vendor ecosystem with standards like IHE, openEHR, and FHIR.
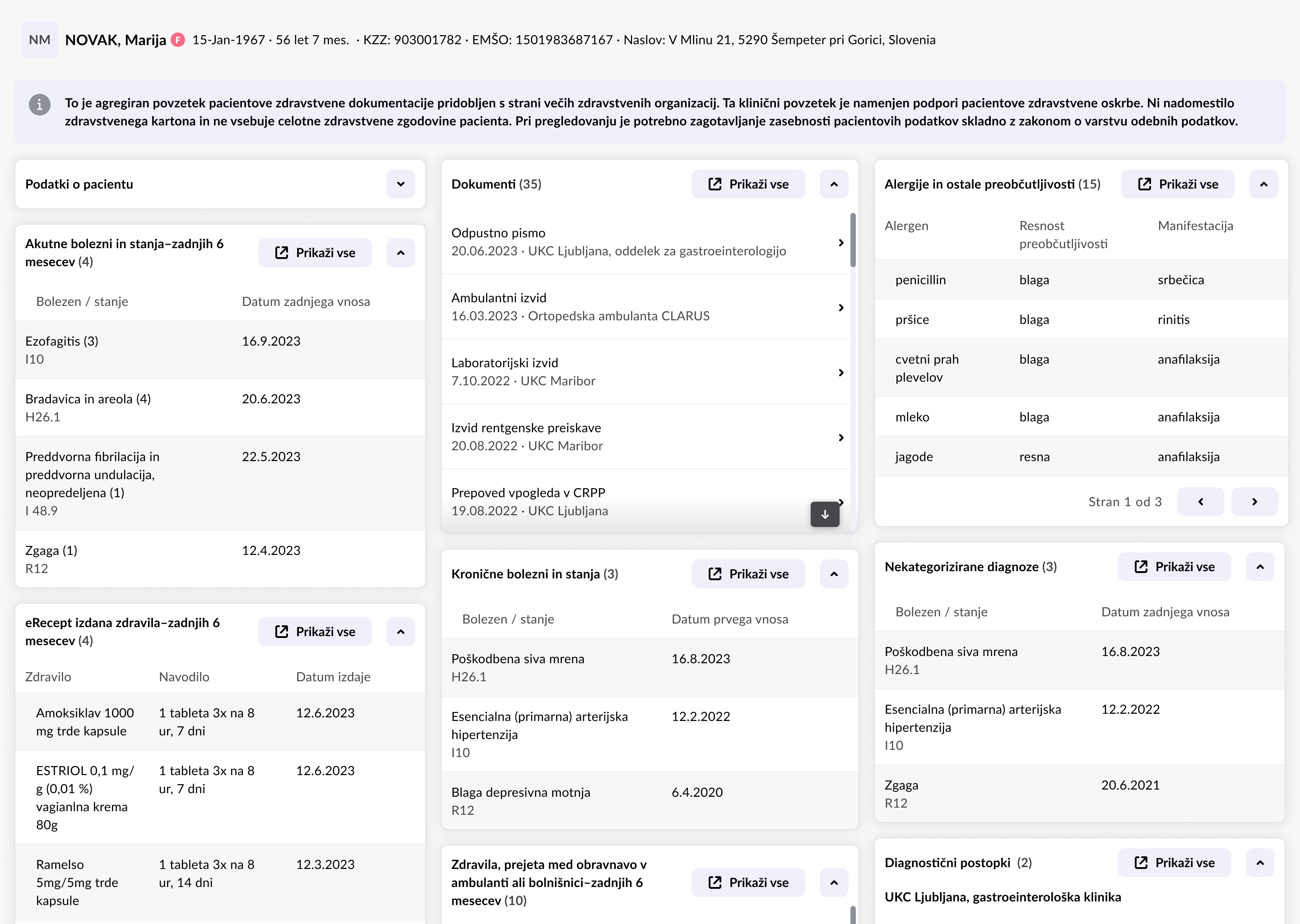
The Central Registry of Patient Data (CRPD) is a unified system for collecting and exchanging health data about patients in Slovenia. It is intended for all healthcare providers, and its purpose is to enable the electronic exchange of health data between healthcare providers so that the data is accessible to all who treat patients.
What were the limitations and challenges?
Since the initial implementation of the CRPD over 10 years ago, technology and healthcare demands have evolved significantly, exposing the limitations of the current system. Key issues include reliance on proprietary technology, inconsistent integration efforts, and hurdles from vast amounts of unstructured healthcare data. This lack of cohesion hinders the seamless integration of critical healthcare data, impeding collaborative efforts and the system's ability to adapt to evolving healthcare needs.
Some of the main obstacles are:
- Outdated technology: the eHealth system faces constraints due to reliance on proprietary technology that is over 15 years old, hindering scalability and interoperability.
- Disparate APIs: system components operate with disparate APIs, lacking standardisation, leading to inconsistencies and complicating integration efforts.
- Authentication and authorisation: the system's security measures rely solely on user roles, and data access often requires navigating through multiple clicks, contributing to inefficiencies.
- Inconsistencies in integration: successful integration using CRPD's APIs coexists with persistent inconsistencies across different healthcare providers. Varying displays of CRPD information and diverse implementations by EMR vendors contribute to a lack of standardisation.
- Unstructured healthcare data: the eHealth system is coping with vast amounts of unstructured data, including clinical notes and narrative reports. This unstandardised information poses challenges for clinicians in accessing and comprehending data efficiently.
- Impacts on clinicians: the time-consuming task of navigating through unstructured documents directly impacts clinicians' ability to access critical information swiftly at the point of care, affecting decision-making processes.What do recent upgrades bring?
What do recent upgrades bring?
The Slovenian Ministry of Health (MoH) implemented a platform-based structure, separating standardised data management from individual applications. The approach eliminates interoperability barriers, making it possible for the MoH to build new use cases or connect applications. Interoperability is now a feature of the CRPD platform, fostering a multi-vendor ecosystem using healthcare standards like IHE, openEHR, and FHIR.
Moving to a standardised and vendor-neutral approach based on FHIR R4 is a major step in advancing Slovenia's national EHR.
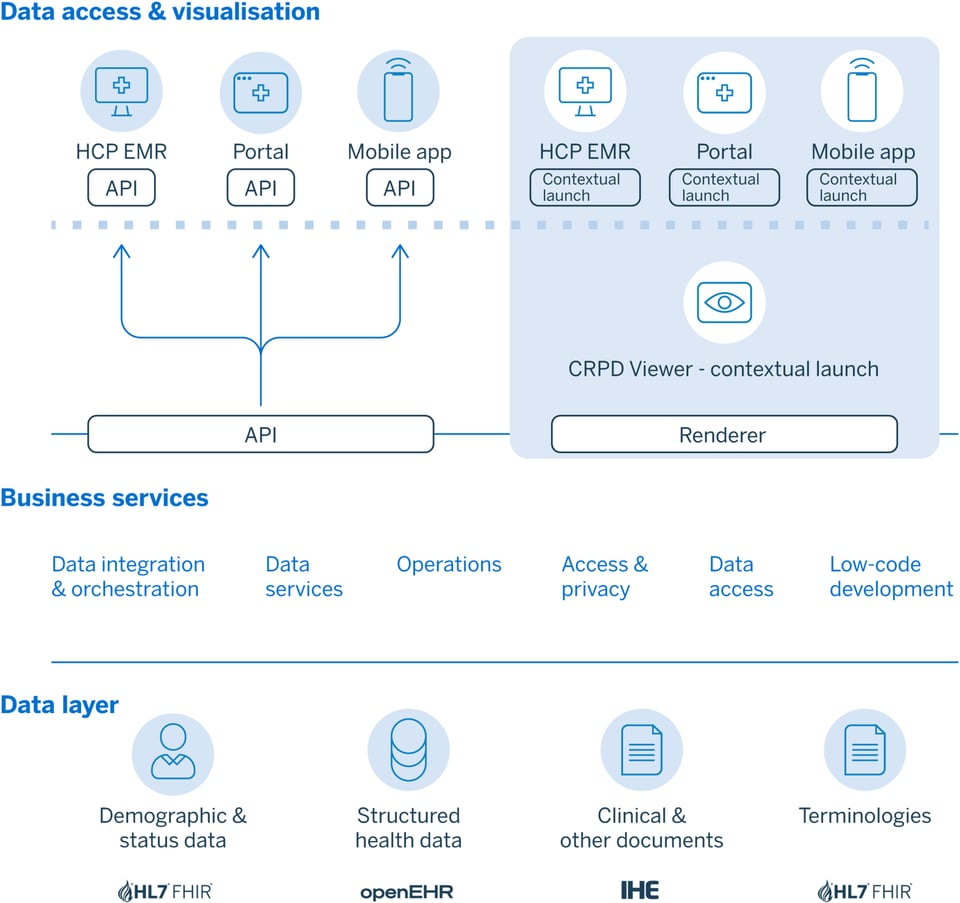
The adoption of HL7 FHIR R4 enhances CRPD, fostering seamless data exchange and positioning it as a harmonised hub for enriched data from diverse governmental sources It also introduces profiled resources including Patient, Location, Practitioner, PractitionerRole, and others that enrich data representation.
A national HL7 FHIR R4 terminology server ensures standardised terminologies, enhancing interoperability and data consistency.
The transition from API-based integration to a context launch model streamlines UI integration. It allows embedding CRPD's interface inside local EHR systems, enhancing consistency, reducing third-party vendor burdens, and facilitating central management. The use of low-code tools enables prompt response to increasing changes in healthcare.
Adoption of Attribute-Based Access Control (ABAC) offers nuanced control over data access and enhances security and privacy. It allows for fine-grained access control, taking into account various attributes, such as user identity, purpose of access, time, and location, when determining access permissions.
CRPD also encourages innovation through low-code development, facilitating alignment with eHealth systems. The national specialty groups use openEHR to design specific care pathways, enhancing compatibility and the national patient record.
The integration of Natural Language Processing extracts clinical codes from unstructured documents, enhancing healthcare analytics and clinical decision support.
The collaboration with the National Public Health Institute offers API services for advanced analytics on infectious diseases, vaccinations, allergies, and rare diseases, emphasising population health monitoring.
A bold leap into the future
The adoption of the CRPD has sparked a transformative shift in the Slovenian healthcare system, elevating efficiency, patient-centreed care, safety measures, and fostering a culture of collaboration and innovation within the healthcare landscape. As Slovenia continues to embrace technological advancements, the future holds promise for further innovation, data sharing, and improved patient care within its national EHR ecosystem.