ehealth
The Optimisation of Hospital Admission by Digitalising Assessment Forms
Clinical assessment forms are a part of clerking for patients during processing. These forms evaluate a patient’s physical condition and prognosis based on information gathered from physical and laboratory examinations and the patient’s medical history. This process is time-consuming – in order to obtain all the necessary patient information, NHS medical teams in the UK need to log-in to several hospital systems and fill in more than 10 clinical forms afterwards for each admission. Some data need to be calculated by hand prior to filling in the form, and this unnecessarily increases the workload of medical teams. Next, the data collected by the paper forms need to be kept in the patient’s health records, or filled into the hospital’s IT systems. This again takes time, and increases the possibility of errors when transcribing the data.
That is why the digitalisation of clinical forms is necessary to optimise the admission process in hospitals, and to lower the risk of errors. There are many different solutions available for digitising the paper forms. Some of them support optical character recognition from paper. The idea is very simple. You scan the paper form, and the solution automatically converts and displays it on a screen. All you have to do then is to bind the input fields to the values on the database. Options on how to do that vary from solution to solution, and can be very complicated.
This is still a viable solution, especially when you want to get all the data that has already been filled into the database, such as demographics, weight, and other pieces of information, which can be used repeatedly. This is much easier than manually editing the data, but it can present issues if the paper form is only partially filled in, or if some of the data is hard to read. Another problem with this approach is that when filling in the paper form, the data presentation can be completely different from the electronic version on a computer or a tablet.
Furthermore, some things are important to show on paper, but are not that important for computers. For example, many forms contain the actual procedure on how to fill in the form. This is sometimes a necessary part of the form. For computers, this information should not be always visible on the screen – only when users want to see it. Such text may include instructions, guidelines, or external links. Additionally, paper forms do not change when values are written on them, but digital forms are adaptable, according to the data about the patient. For instance, if a body mass index is below 20, then the digital form can offer options for additional data to be added. Also, digitising a paper form is just one part of the digitalisation process. The data collected need to be stored in a structured way for re-use in other hospital contexts, or in another healthcare organisation.
Malnutrition Universal Screening Tool (MUST)
One of these examples is the Malnutrition Universal Screening Tool (MUST). This is the most commonly used nutritional screening tool in all care settings in the UK (e.g. in 85% of hospitals and 92% of care homes), and is also common in other countries.[1] The MUST screening tool needs to be used upon admission, and repeatedly during a patient’s stay in hospital – on a weekly basis. Care workers follow a five-step procedure to identify adults who are malnourished, at risk of malnutrition (undernutrition), or obese. Additionally, the tool includes management guidelines which can be used to develop care plan. It is for use in hospitals, community and other care settings, and can be used by all care workers.[2]
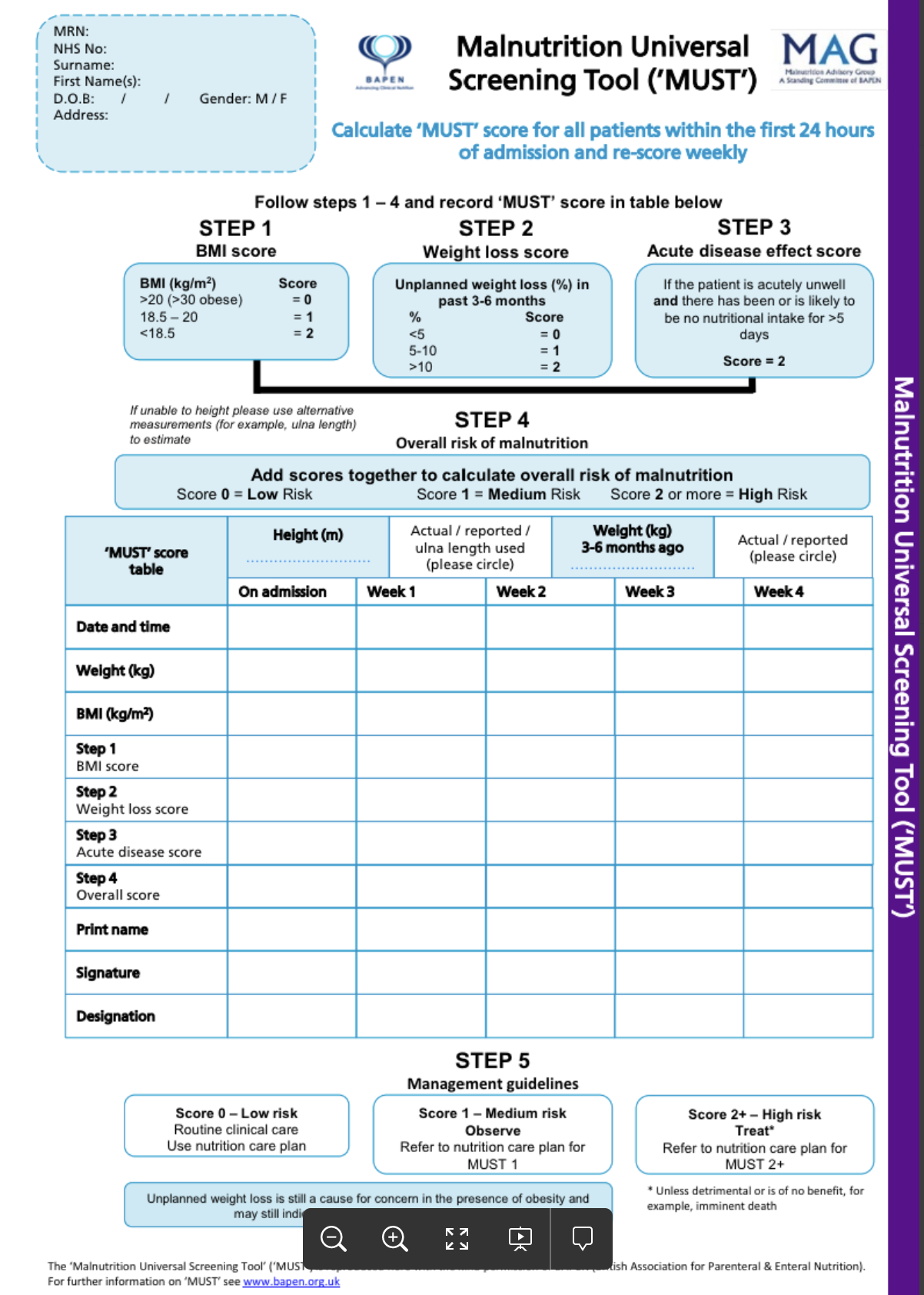
Here is an example a paper MUST form, which can be used only four times before another form is required.
In addition to filling out the patient’s data on the MUST form, the medical teams have to calculate the body mass index (BMI) every time. When filling in a paper form, the care person must calculate the BMI by hand, with a calculator or a mobile phone. Additional complications occur if the height of a patient is unknown or cannot be measured (for example, if a patient is unable to stand or is unconscious). In this instance, the height must be calculated using the ulna length, or a similar height prediction algorithm. The BMI also needs to be calculated using the metric system, which poses another challenge in the UK, since not all people know their height in metric. These conversions and calculations take time and increase the possibility of data errors. On a screen this can of course be done automatically, including the conversions from imperial to metric units – the whole admission process is done in much less time, and with much less risk of making mistakes during data entry.
.png?width=717&name=MUST_forma_2021_02_18%20(2).png)
Here is an example of a digital MUST form.
The MUST form is just one of the many examples where digital forms present the opportunity of decreasing the workload of medical teams. Transferring data from paper to digital clinical forms that are built with a low-code development environment on top of an openEHR digital health platform have several benefits:
- A better user experience and improved processes: the form structure and the clinical process do not need to fit the paper format – they can be optimised to suit the requirements of a process, or the needs of the medical teams.
- Saving time and reducing the workload of medical teams: there is no need for conversions or time-consuming, manual calculations (e.g. BMI). Additionally, it is possible to have a predefined value-set of options, and get the data from a database, so that the user does not have to fill them in each time (for example, the height of a patient) when doing a reassessment.
- Clinical process optimisation: changing a paper form to suit the processes in hospitals better takes a lot of time, whereas changing digital forms can be done in days.
- 360-degree patient overview: currently, medical teams need to access several different applications to obtain all the relevant patient data. Digital forms can be embedded in existing applications, or a modular and composable clinician portal and context-aware patient chart that enable fast access to key patient information when and where needed.
- Increased patient safety: a reduction of errors in manual calculations and data loss when entering the data from paper forms to hospital IT systems.
- Increased patient data privacy: entered data can be only accessed by authorised hospital personnel.
- Data quality: the data which is entered into the form is structured in an interoperable way, and can be used for other purposes in the hospital.
- Fast and agile form development: the form building process is fast, and changes in production can be implemented immediately. Furthermore, the forms can be developed without any knowledge of coding, and in collaboration between medical teams and IT personnel.
The benefits of digital clinical forms have already been well-proven in practice. See how the Somerset NHS Foundation Trust in the UK was able to rapidly create, customise, deploy, and improve COVID-19 digital forms in less than three weeks here:
|
Register for a free webinar ‘COVID-19 rapid response: A Data-Platform Approach’ recording with Martyn Strawbridge, Deputy CNIO, and Mark Hunt, IT Development Manager. |
1: C A Russell and M Elia: NUTRITION SCREENING SURVEY IN THE UK AND REPUBLIC OF IRELAND IN 2011. A Report by the British Association for Parenteral and Enteral Nutrition (BAPEN), accessed 8 December 2020 at: https://www.bapen.org.uk/pdfs/nsw/nsw-2011-report.pdf.
2: BAPEN: Malnutrition Universal Screening Tool, Accessed 15 December 2020 at: https://www.bapen.org.uk/pdfs/must/must_full.pdf